Obstructive Sleep Apnoea Treatment: CPAP vs. MAD Devices
CPAP and MAD devices can both be effective for treating sleep apnoea, depending on the individual
5 minute read
If you snore loudly or wake up choking in the night, you might be experiencing obstructive sleep apnoea. This is a common sleep disorder, but one that can have serious effects on physical and mental health if it’s not treated.
If your dentist or doctor diagnoses obstructive sleep apnoea, they may discuss a range of treatment options, depending on the cause and severity of your condition. The two most common approaches use Continuous Positive Airway Pressure (CPAP) and Mandibular Advancement Device (MAD) devices.
Read this comparison of CPAP vs MAD devices for sleep apnoea treatment and make an appointment with our dentists in Kelmscott to discuss your options. We’ll help you find the right treatment to start sleeping soundly and lower your health risks.
What is obstructive sleep apnoea (OSA)?
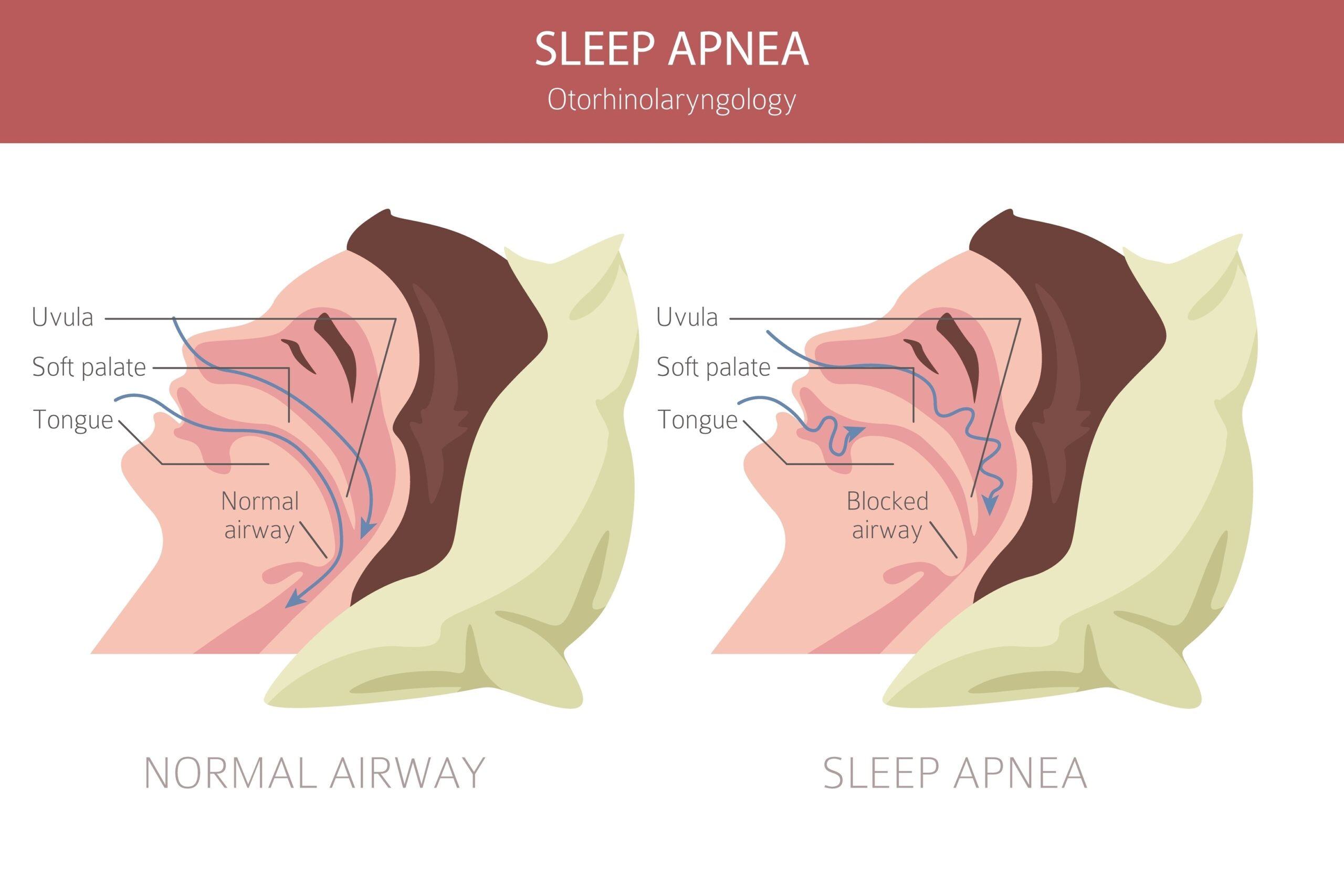
Obstructive sleep apnoea (OSA) is a breathing-related sleep disorder that can occur when the muscles in your throat relax during sleep and the airway becomes blocked or restricted, preventing you from breathing normally.
According to a 2017 systematic review, sleep apnoea affects between 9% to 38% of adults worldwide.
If your brain detects low oxygen levels in your blood, it will send signals to your body to forcibly wake you up and clear the obstruction. This can cause you to wake up suddenly, sometimes gasping for breath.
These events are so brief that many people don’t remember waking up in the night. OSA can occur hundreds of times throughout the night, which prevents people from getting the restful sleep they need.
OSA symptoms
You might not be aware of waking up in the night unless someone else tells you. Other signs that you might have obstructive sleep apnoea can include:
- Loud snoring or breathing
- Gasping for air during sleep
- Morning headaches
- Dry mouth
- Tiredness during the day
- Irritability
- Difficulty remembering or concentrating
OSA risk factors
Anyone can experience OSA, but some factors will increase your risk and include:
- Being overweight
- Being a male over 30 years of age
- Having a thick neck or narrow throat
- Smoking or alcohol use
- Sedatives and tranquilisers
- Nasal congestion
- Certain medical conditions, including congestive heart failure, high blood pressure and type 2 diabetes
- Family history of sleep apnoea
Health risks of untreated sleep apnoea
Sleep disturbances caused by obstructive sleep apnoea can have many serious complications that can get worse over time if it isn’t treated. These risks include:
- Increased risk of motor vehicle accidents and other accidents due to tiredness and concentration lapses
- Decreased performance at work or school due to tiredness and problems with memory and concentration
- Increased risk of heart problems, high blood pressure, type 2 diabetes and other medical conditions due to low blood oxygen levels
- Complications with anaesthesia during surgery
- Mood and behaviour problems, such as irritability or depression
- Reduced quality of life for yourself and people you live with due to tiredness and fatigue
Treatment options for obstructive sleep apnoea
If you think you might have obstructive sleep apnoea or another sleep disorder, talk to your dentist about your concerns. They will be able to refer you to a sleep specialist to conduct an overnight sleep study and diagnose the condition.
Sleep apnoea is measured using a system called the apnea-hypopnea index (AHI). AHI measures the number of times you stop breathing per hour during sleep.
Obstructive sleep apnoea is classified by severity:
- Severe obstructive sleep apnoea means that your AHI is greater than 30 (more than 30 episodes per hour)
- Moderate obstructive sleep apnoea – an AHI between 15 and 30
- Mild obstructive sleep apnoea means – an AHI between 5 and 15
Depending on how severe your sleep apnoea is, a range of treatment options may be recommended. These can include:
- Lifestyle changes: for some mild cases, taking steps to lower your risk profile – such as losing weight, improving your sleep posture, or avoiding smoking and alcohol – will reduce the severity of symptoms or alleviate them together.
- CPAP therapy: breathing pressurised air through a face mask to keep the airway open during sleep, often recommended for moderate to severe OSA.
- MAD device: wearing a custom oral appliance at night to hold the throat open and prevent breathing interruptions, often recommended for mild to moderate OSA.
- Surgery: sometimes necessary for severe OSA cases when other treatments are not successful.
If you’re not getting enough sleep and want to discuss CPAP or MAD devices for sleep apnoea, call our friendly team today on (08) 9495 7999.
Lifestyle changes
Weight loss has long been considered an effective way to address symptoms of OSA. Studies suggest that a 10% reduction in weight leads to a 26% improvement in sleep disruption. Losing weight also improves overall health, quality of life, and likely decreases daytime sleepiness.

Changing sleep posture to sleep on your side rather than your back is also considered an effective way to alleviate OSA, as does refraining from smoking, alcohol and medications that suppress the central nervous system and exacerbate OSA.
CPAP therapy
Continuous Positive Airway Pressure (CPAP) involves the use of a machine and face mask to deliver a steady stream of air into the airway during sleep. This air is at slightly higher pressure than the air around it, which helps to keep the airways open and prevent obstructions.
Benefits of CPAP therapy
- High success rate and long-term adherence
- Effective for moderate to severe OSA
- Suitable for a wide range of patients
Challenges of CPAP therapy
- Some people find the mask uncomfortable or obtrusive
- Lack of portability
- High maintenance requirements
MAD devices
A Mandibular Advancement Device or Splint (MAD or MAS) is an oral appliance provided by a dentist to fit over your teeth, similar to a mouthguard. It’s designed to bring your jaw and tongue slightly forwards during sleep, which helps to open the airway and prevent blockages and sleep apnoea.
Benefits of MAD devices
- Less invasive than CPAP therapy
- Portable and convenient
- Effective for mild to moderate OSA
Challenges of MAD devices
- May cause jaw discomfort or TMJ pain
- May not be effective for severe OSA
- May be less suitable for older patients or those with missing teeth
CPAP vs. MAD devices: A side-by-side comparison
Reviews of multiple studies have found that CPAP and MADs are both effective at reducing symptoms of obstructive sleep apnoea in patients, but this can vary from person to person according to the severity of symptoms. A number of factors need to be considered when deciding which could be the best solution for you.

Comfort and ease of use
Both devices have an adjustment period, but CPAP devices may take longer for some people to get used to. Some may find the mask too uncomfortable to wear, or may find the noise produced by the CPAP machine distracting, though it doesn’t bother everyone.
MAD appliances are less invasive and are custom made to fit comfortably over the teeth, but they may cause tension or discomfort in the jaw and joints for some.
Effectiveness
Both devices have been found to be similarly effective at treating mild to moderate OSA and improving related symptoms, but MAD devices have more limited effectiveness at treating more severe OSA.
CPAP isn’t effective in all cases, as some people may find the treatment uncomfortable or may struggle to use it as advised, preventing them from sleeping soundly.
Whichever approach is used, a follow-up sleep study is recommended to check that the device is working effectively or to make any adjustments needed.
Portability and convenience
If you need a device you can take with you when travelling, MAD devices are more portable and convenient than CPAP machines. CPAP devices also require a power source and produce a level of noise that could be disruptive to other people. CPAP machines have evolved over time and it’s suggested that newer models generally produce less noise.
Cost and maintenance
Both types of devices have initial and ongoing costs to consider. In many cases, it may be necessary to continue using the device for the long term, even if OSA symptoms improve, to prevent the problem from returning.
CPAP generally involves higher maintenance costs to clean and service the machine and replace parts as needed, but it may be possible to claim some of these costs on your health insurance, depending on your cover.
MAD devices are custom made and provided by your dentist or purchased over-the-counter. A custom device costs more, but it offers a perfect fit to prevent discomfort and problems. You can ask your dentist about their payment plans to help make the cost easier to manage.
Who is a good candidate for CPAP or MAD devices?
You may be suitable for either approach if you have mild to moderate obstructive sleep apnoea, but each has its restrictions.
- CPAP offers maximum airway support, making it suitable for some people with severe OSA. It also doesn’t require that you have strong teeth and jaws. However, not everyone can tolerate CPAP machines or finds them convenient.
- MAD devices can be easier and more comfortable to use, but they offer less airway support that can make them less effective for more severe OSA. They also rely on the teeth and jaws for support, so may not be an option if you have weak or missing teeth or a sensitive jaw joint muscles.
- In some situations, your dentist or sleep physician may recommend trying a combined approach using both techniques.
Getting the most from your treatment
To get the maximum benefit from CPAP or MAD therapy, it’s important to adopt lifestyle changes known to lower your risk factors for OSA and avoid activities or substances that can worsen its symptoms. This may include:
- Losing weight
- Getting regular exercise
- Sleeping on your side rather than flat on your back
- Avoiding smoking
- Avoiding alcohol 4 to 6 hours prior to bedtime
- Avoiding sedatives
- Seeking treatment for related conditions such as nasal congestion

Talk to our dentists in Kelmscott
If you or someone in your family is struggling with obstructive sleep apnoea, our dentists at Kelmscott Dental could help. We work with sleep specialists to determine the cause and most suitable treatment options for OSA to help you and your loved ones sleep soundly.
To find out more or book a consultation, call (08) 9495 7999 or book online. We welcome patients from all nearby areas, including Armadale and Gosnells.
References
1. https://www.mayoclinic.org/diseases-conditions/sleep-apnea/
2. Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev 2017;34:70-81.
3. https://www.racgp.org.au/getattachment/d5d13af4-d28e-445c-b388-e5cba6cb442a/Mandibular-devices-for-obstructive-sleep-apnoea.aspx
4. Pattipati M, Gudavalli G, Zin M, Dhulipalla L, Kolack E, Karki M, Devarakonda PK, Yoe L. Continuous Positive Airway Pressure vs Mandibular Advancement Devices in the Treatment of Obstructive Sleep Apnea: An Updated Systematic Review and Meta-Analysis. Cureus. 2022 Jan 31;14(1):e21759. doi: 10.7759/cureus.21759. PMID: 35251830; PMCID: PMC8890605.
5. White DP; Shafazand S. Mandibular advancement device vs CPAP in the treatment of obstructive sleep apnea: are they equally effective in short term health outcomes? J Clin Sleep Med 2013;9(9):971-972.
6. Mitchell, L.J., Davidson, Z.E., Bonham, M., O’Driscoll, D.M., Hamilton, G.S. and Truby, H. (2014). Weight loss from lifestyle interventions and severity of sleep apnoea: a systematic review and meta-analysis. Sleep Medicine, 15(10), pp.1173–1183. doi:https://doi.org/10.1016/j.sleep.2014.05.012.
Obstructive Sleep Apnea (OSA) Treatment & Management: Approach Considerations, Nasal CPAP Therapy, BiPAP Therapy. (2021). eMedicine. [online] Available at: https://emedicine.medscape.com/article/295807-treatment


